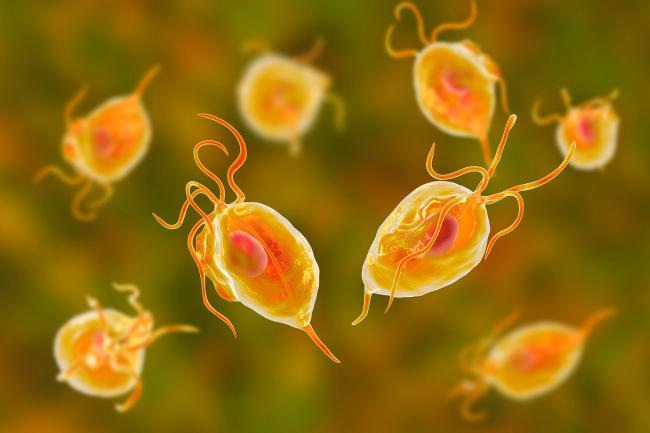
Professor Hall first began working on malaria through a stroke of serendipity. After joining the Sanger Institute, where he was brought in to work on the fungal pathogen Aspergillus fumigatus, the chance arose to work on the Plasmodium genome. As the only person working on a eukaryotic pathogen at the time, Hall was the perfect candidate.
“It was a flagship genome project at that time,” says Hall. “Then, it was the biggest threat to human health by an infectious disease in the world.”
Malaria is still the sixth biggest cause of death overall in low income countries. “It was a fascinating organism to work on,” Hall enthuses as he recounts his early work. “It's such a highly specialised pathogen. It can enter your bloodstream and in a matter of minutes find your liver cells. Different genes then allow it to infect your red blood cells, which is when you start to show symptoms. Other forms are designed to affect mosquito cells, where it has its sexual cycle.”
Those trying to fight back against malaria face a difficult task because the malaria parasite has developed a cloak and dagger approach to infecting its human host. Normally, the immune system fights invaders by detecting antigens on the surface of infected cells. Plasmodium, however, can shuffle through multiple versions of these surface antigens and evade the immune system for months at a time.
This is how the parasite manages to survive over the long dry months when mosquitoes are not around. It’s also one of the reasons malaria is so devilishly difficult to treat, and renders many attempts at making vaccines ineffective. Known as antigenic cycling, it’s something that Hall’s early genome work was able to get to the bottom of.
“One of the most exciting things we discovered was the structure of the chromosomes,” says Hall. “It turns out the genes that allow Plasmodium to do this antigenic cycling exist at the telomeres. They have a very specific orientation which allows recombination to change which of the genes is at the active telomere, and little cassette modules of different domains which can, through rare recombination events, generate new genes.”