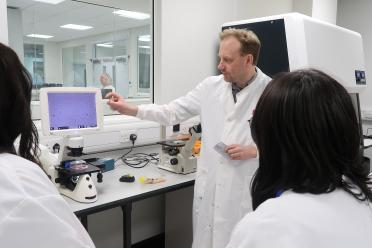
The pioneering nanosurgical platform has been developed by University of Leeds scientists, underpinned by training and advice on single-cell science from the Earlham Institute.
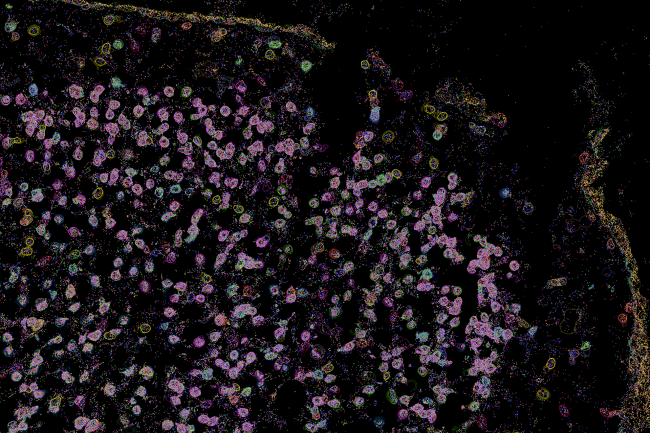
It means that, for the first time, researchers can see how individual living cancer cells react to treatment and change over time – providing vital understanding that could help doctors develop more effective cancer medication.
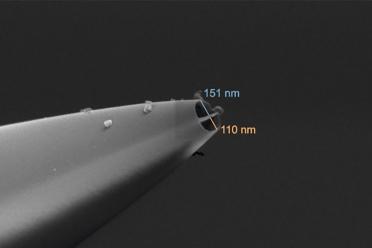
The tool has two nanoscopic needles, meaning it can simultaneously inject and extract a sample from the same cell, expanding its potential uses. And the platform’s high level of semi-automation has sped up the process dramatically, enabling scientists to extract data from many more individual cells, with far greater accuracy and efficiency than previously possible, the study shows.
Currently, techniques for studying single cells usually destroy them, meaning a cell can be studied either before treatment, or after.
This device can take a “biopsy” of a living cell repeatedly during exposure to cancer treatment, sampling tiny extracts of its contents without killing it, enabling scientists to observe its reaction over time.
During the study, the multi-disciplinary team, featuring biologists and engineers, tested cancer cells’ resistance to chemotherapy and radiotherapy using glioblastoma (GBM) - the deadliest form of brain tumour - as a test case, because of its ability to adapt to treatment and survive.
One of the paper’s corresponding authors, Dr Lucy Stead, Associate Professor of Brain Cancer Biology in the University of Leeds’ School of Medicine, said: “This is a significant breakthrough. It is the first time that we have a technology where we can actually monitor the changes taking place after treatment, rather than just assume them.
“This type of technology is going to provide a layer of understanding that we have simply never had before. And that new understanding and insight will lead to new weapons in our armoury against all types of cancer.”
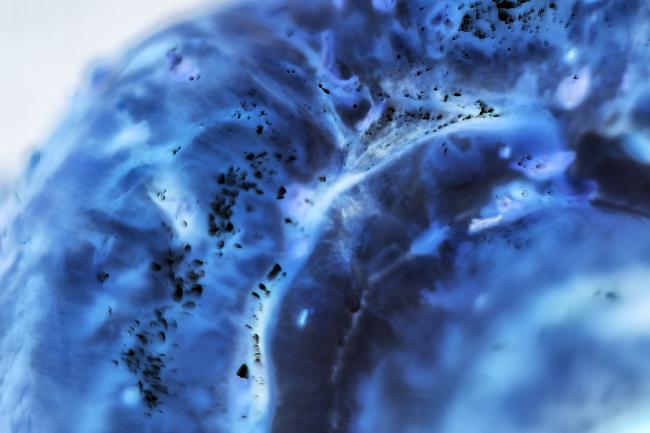
She added: “GBM is the cancer in most need of those new weapons because in 20 years there has been no improvement in survival in this disease.
“It is lagging behind so much and we think that is because of the highly ‘plastic’ nature of these tumours – their ability to adapt to treatment and survive it.
“That is why it is so important that we can dynamically observe and characterise these cells as they change, so we can map out the journey these cells can take, and subsequently find ways to stop them at every turn. We simply couldn’t do that with the technologies that we had.”
Dr Stead leads the Glioma Genomics research group at the Leeds Institute of Medical Research at St James's Hospital, which is focused on trying to cure GBM brain tumours. She added: “This technology could be transformative for this particular cancer, helping us finally identify effective treatments for this awful, incurable disease.”